Anthrax, Arsenic and Old Lace
by Sally Fallon Morell, Nourishing Traditions
August 22, 2020
Anthrax is an infection caused by the bacterium Bacillus anthracis. It can occur in four forms: skin, lungs, intestinal and injection. Symptoms begin between one day to over two months after the infection is contracted. The skin form presents as a characteristic black blister.
The inhalation form presents with fever, chest pain and shortness of breath. The intestinal form presents with diarrhea which may contain blood, abdominal pains, nausea and vomiting. The injection form presents with fever and an abscess at the site of drug injection.
Anthrax is spread by contact with the bacterium’s spores, which often appear in infectious animal products. Contact is by breathing, eating or through an area of broken skin. Anthrax does not typically spread directly between people or animals—in other words, it is not contagious.
Although a rare disease, human anthrax, when it does occur, is most common in Africa and central and southern Asia. Anthrax infection on the skin is known as hide-porter’s disease. Historically, inhalational anthrax was called wool sorters’ disease because it was an occupational hazard for people who sorted wool.
Bacillus anthracis is a rod-shaped, Gram-positive, facultative anaerobic bacterium about 1 by 9 μm in size. The bacterium normally rests in spore form in the soil, and can survive for decades in this state.
Today, this form of infection is extremely rare in advanced nations, as almost no infected animals remain. In November 2008, a drum maker in the United Kingdom who worked with untreated animal skins died from inhalation anthrax.
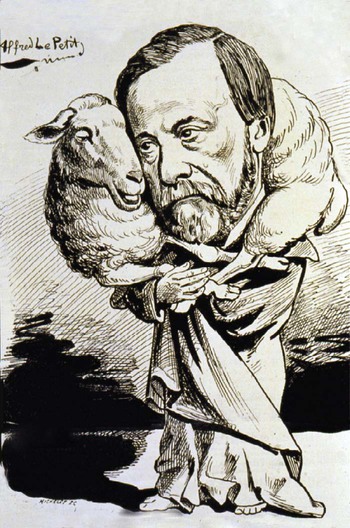
Anthrax posed a major economic challenge in France and elsewhere during the 19th century. Sheep were particularly vulnerable, and national funds were set aside to investigate the production of a vaccine. Louis Pasteur dedicated several years to this quest after Robert Koch, his German rival, claimed discovery of the causative agent, Bacillus anthracis.
 In May 1881, Pasteur performed a public experiment at Pouilly-le-Fort to demonstrate his concept of vaccination. He prepared two groups of twenty-five sheep, one goat and several cattle. The animals of one group were twice injected with an anthrax vaccine prepared by Pasteur, at an interval of fifteen days; the control group was left unvaccinated. Thirty days after the first injection, both groups were injected with a culture of live anthrax bacteria. All the animals in the unvaccinated group died, while all of the animals in the vaccinated group survived.
In May 1881, Pasteur performed a public experiment at Pouilly-le-Fort to demonstrate his concept of vaccination. He prepared two groups of twenty-five sheep, one goat and several cattle. The animals of one group were twice injected with an anthrax vaccine prepared by Pasteur, at an interval of fifteen days; the control group was left unvaccinated. Thirty days after the first injection, both groups were injected with a culture of live anthrax bacteria. All the animals in the unvaccinated group died, while all of the animals in the vaccinated group survived.
This apparent triumph, widely reported in the local, national and international press, made Pasteur a national hero and ensured the acceptance of vaccination in the practice of medicine. That’s the official story.
Now, let’s examine it more closely.
Pasteur’s public triumphs look different when we compare the glowing newspaper reports with his private notebooks, analyzed by Gerald L. Geison in his book The Private Science of Louis Pasteur. Anthrax was indeed a major problem in livestock in France during the nineteenth century, especially among sheep, and the efforts to find a vaccine enticed Louis Pasteur and other scientists of his day into a fiercely competitive race for the glory and the gold.
Pasteur promoted the germ theory, widely disputed at the time, that microbes caused most if not every disease. The germ theory allowed scientists to envisage a quick fix to disease with a vaccine containing a weakened or attenuated form of the bacteria—similar to the then-common idea that a little bit of poison could make you immune to a larger dose.
Reading about these early attempts to find a vaccine for anthrax conjures up images of Monty Python and the Ministry of Silly Science. Some scientists attempted “attenuation” by subjecting the microbe to a poison, potassium bichromate, or carbolic acid, a disinfectant. Another thought he could create an attenuated vaccine by heating the blood of infected animals and injecting it into non-infected ones. Some favored boiling the bacteria in chicken broth, others in urine. One of Pasteur’s colleagues tried to “enfeeble” anthrax cultures by exposing them to gasoline vapors. Pasteur attempted to destroy the virulence of the anthrax bacillus by subjecting it to “atmospheric oxygen,” science-speak for air—all of these theories pursued with John Cleese-like gravitas.
Unfortunately for these would-be heroes, none of the ideas worked very well. Pasteur’s rival, a veterinarian named Touissant, focused on heated blood, which he initially claimed could serve as an effective vaccine. Later, however, he found that the results were inconsistent, even killing experimental animals, and began to add carbolic acid, which did not meet with expectations either. In his notebooks, Pasteur expressed frustration that his experiments with rabbits, Guinea pigs, monkeys and dogs gave such inconclusive results. The magic vaccine was elusive, and Pasteur had “exceptionally little experimental basis for announcing the ‘discovery’ of an anthrax vaccine in January 1880” (Geison, page 167). Pasteur made a similar announcement in February 1881, and in March he reported successful results in preliminary tests on sheep. As Geison reports, “. . . the boldly confident tone of Pasteur’s public reports exaggerated the actual results to date of his experiments with the new vaccine. In fact, the results of his tests remained ‘decidedly inconclusive’” (Geison, page 170). Yet Pasteur, to the dismay of his co-workers, “impulsively” accepted the challenge of Pouilly-le-Fort and signed the detailed and demanding protocol of experiments on April 28, 1881.
The other problem was that try as he may, Pasteur was unable to make animals sick by injecting them with the microbe he associated with the disease he was studying, such as anthrax or rabies. In the case of anthrax, to make healthy animals sicken and die, he had to inject them with “virulent anthrax.” Pasteur made “pathogenic” microbes more virulent by what he called “serial passage” of the organism through other animals—in the case of anthrax he used Guinea pigs, injecting them with the microorganism he associated with anthrax, then sacrificing the animal and injecting its blood or tissue, possibly mixed with poisons such as carbolic acid or potassium bichromate, into another animal; this process was repeated through several Guinea pigs. In this way he came up with what he called “virulent anthrax.” (For rabies, he was able to produce the symptoms of disease by injecting “cerebral matter. . . extracted from a rabid dog under sterile conditions and then inoculated directly onto the surface of the brain of a healthy dog through a hole drilled into its skull.” This treatment did sometimes make dogs foam at the mouth and die (Geison, page 189).
In the midst of his frustrating anthrax experiments, Pasteur was enticed by the Academy of Medicine into making the celebrated demonstration at Pouilly-le-Fort. With his rival Touissant (a mere vet, not even a true scientist!) breathing down his neck, his enemies made him sign the protocol of an experiment they judged impossible of success.
Geison makes much of the fact that Pasteur deliberately deceived the public about the nature of the vaccine he used, although there was no particular reason for doing so. The protocols did not specify the kind of vaccine that Pasteur would inoculate into the animals. Pasteur was equally cagey earlier about how he made his vaccine for chicken cholera.
The key point: unlike all his early experiments, the trials at Pouilly-le-Fort worked perfectly! All the vaccinated sheep lived and all the unvaccinated sheep died. A triumph!
One has the right to ask: did Pasteur cheat? After all, the stakes were high, and Pasteur’s notebooks indicate that he was sometimes dishonest, even unsavory. He was also extremely aggressive in defending his interests, having destroyed several opponents with manipulation and rhetoric.
The death of all the unvaccinated sheep is easy to explain. He used “virulent anthrax,” in other words, he poisoned them. What about the vaccinated sheep that lived? All of them. Did he inject them with “virulent anthrax” or merely anthrax, with which he could never succeed in killing animals. As the French would say, “Il y avait quelque chose de louche.” Something fishy was going on.
After the trial, requests for supplies of his anthrax vaccines flooded Pasteur’s laboratory. But Pasteur and also his assistants remained surprisingly reticent to disclose any details about the type of vaccine they used. Nevertheless, Pasteur’s laboratory soon acquired a monopoly on the manufacture of commercial anthrax vaccines, and he aggressively pursued foreign sales. Pasteur and his laboratory enjoyed a net annual profit of 130,000 francs from the sale of anthrax vaccines in the mid-1880s.
The problem was—and another source of suspicion that Pasteur cheated—the vaccine didn’t work. In Pasteur: Plagiarist, Imposter, author R. B. Pearson notes that Pasteur began to receive letters of complaint from towns in France and from as far away as Hungary, of fields littered with dead sheep, vaccinated the day before. According to the Hungarian government, “the worst diseases, pneumonia, catarrhal fever, etc., have exclusively struck down the animals subjected to injection.” An 1882 trial carried out in Turin found the vaccination worthless. In southern Russia, anthrax vaccines killed 81 percent of the sheep that received them.
Gradually use of the vaccine faded. . . but here’s the mysterious thing: the occurrence of anthrax faded also. Today it is a rare disease. So what was causing the death of animals, mostly sheep, during the nineteenth century and why don’t sheep die of anthrax today?
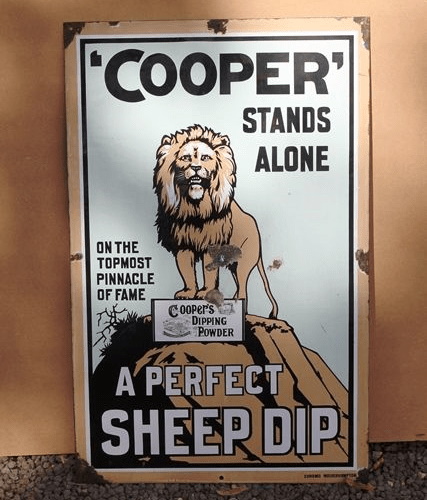 Let us consider sheep dip. The world’s first sheep dip was invented and produced by George Wilson of Coldstream, Scotland in 1830—it was based on arsenic powder. One of the most successful brands was Cooper’s Dip, developed in 1852 by the British veterinary surgeon and industrialist William Cooper. Cooper’s dip contained arsenic powder and sulfur. The powder had to be mixed with water, so naturally agricultural workers—let alone sheep dipped in the arsenic solution–sometimes became poisoned.
Let us consider sheep dip. The world’s first sheep dip was invented and produced by George Wilson of Coldstream, Scotland in 1830—it was based on arsenic powder. One of the most successful brands was Cooper’s Dip, developed in 1852 by the British veterinary surgeon and industrialist William Cooper. Cooper’s dip contained arsenic powder and sulfur. The powder had to be mixed with water, so naturally agricultural workers—let alone sheep dipped in the arsenic solution–sometimes became poisoned.
The symptoms of arsenic poisoning are remarkably similar to those of “anthrax,” including the appearance of black skin lesions. Like anthrax, arsenic can poison through skin contact, through inhalation and through the gastro-intestinal tract. If an injection contains arsenic, it will cause a lesion at the site.
Sheep dips today no longer contain arsenic so anthrax has disappeared—except in developing countries where it is still an ingredient in industrial processes like tanning—hence the 2008 death of the drum maker working with imported skins.
The real mystery is why scientists of the day did not make the connection between anthrax and arsenic. After all, the French knew a thing or two about arsenic—every physician and pharmacist stocked arsenic powder and in Flaubert’s bestselling mid-century novel Madame Bovary, his heroine kills herself by swallowing a handful of arsenic. Flaubert graphically describes the black lesions that mar the beautiful Madame Bovary as she dies—every Frenchman knew what arsenic poisoning looked like. It seems that scientists, vets and physicians were so dazzled by the new germ theory that they could not make the connection of poison with disease.
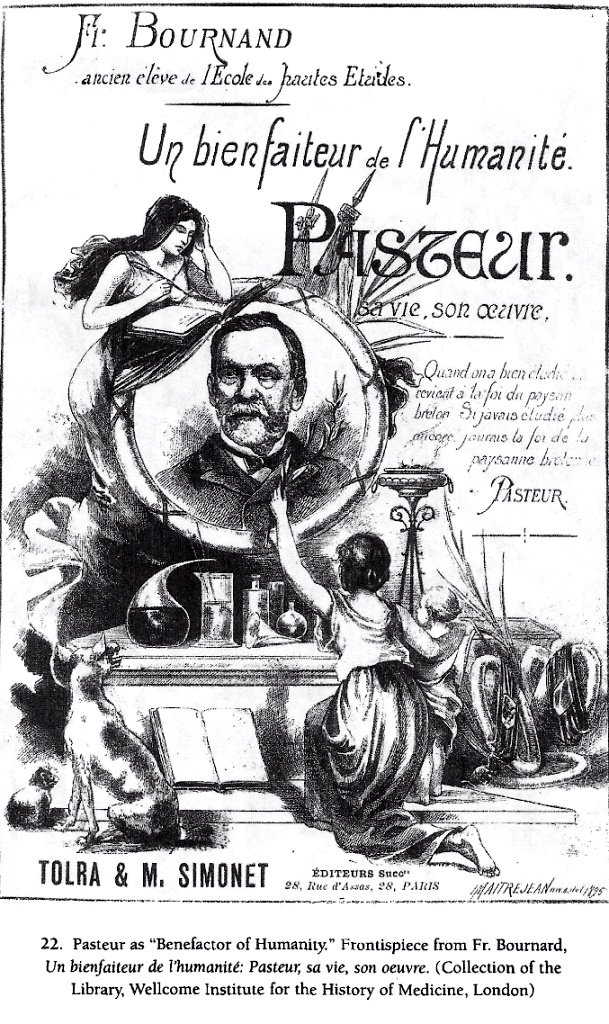 Pasteur died in 1895 and immediately took his place as the premiere saint of medicine, the press featuring engravings that reeked of old lace, showing him as the subject of adulation, his flasks and beakers placed on an altar, a grateful admirer kneeling before them. Science had become the new religion.
Pasteur died in 1895 and immediately took his place as the premiere saint of medicine, the press featuring engravings that reeked of old lace, showing him as the subject of adulation, his flasks and beakers placed on an altar, a grateful admirer kneeling before them. Science had become the new religion.
But Pasteur did not radiate the satisfaction of having saved lives. He spent his last years enfeebled and sad-looking, his faults etched as deep lines of stress and worry around his eyes.
Anthrax faded from public consciousness and anthrax vaccines languished until the famous anthrax letters, sent to well-known members of the media and two senators a couple weeks after 9/11. At least twenty-two people became sick and five died. Genetic testing (not isolation of the bacteria) indicated anthrax spores but no one tested the powders for arsenic.
The attacks revived interest in the anthrax vaccine. According to conventional sources, all currently used anthrax vaccines provoke reactions, such as rash, soreness and fever, and serious adverse reactions occur in about 1 percent of recipients. Rarely used for decades, the vaccine was dusted off for use in the “at risk” category, such as members of the military. Solders get the vaccine in five consecutive doses, with a booster every year.
Mandatory vaccinations for military men were halted in 2004 by a legal injunction which challenged the vaccine’s safety and effectiveness.But after a 2005 FDA report claiming the vaccine was safe, the Defense Department reinstated mandatory anthrax vaccinations for more than two hundred thousand troops and defense contractors.
One last thought: scientists have found that certain bacteria can “bioremediate” arsenic in the soil. These arsenic-resistant and/or accumulating bacteria “are widespread in the polluted soils and are valuable candidates for bioremediation of arsenic contaminated ecosystems.” Nature always has a solution, and in the case of arsenic, the solution is certain ubiquitous soil bacteria. We need to entertain the possibility that the “hostile” anthrax bacteria, first isolated by Robert Koch, is actually a helpful remediation organism that appears on the scene (or in the body) whenever an animal or human encounters the poison called arsenic.

Truth Comes to Light highlights writers and video creators who ask the difficult questions while sharing their unique insights and visions.
Everything posted on this site is done in the spirit of conversation. Please do your own research and trust yourself when reading and giving consideration to anything that appears here or anywhere else.