Are Doctors’ Strikes Really a Disaster for Our Health?
by Dawn Lester, Dawn’s Writings
March 17, 2023
The medical system in the UK, known as the NHS, is currently in crisis and I wholeheartedly agree!
But the real nature of the crisis is not how it is portrayed by the mainstream media, which is demonstrated by a January 2023 BBC article entitled The NHS crisis – decades in the making that states,
“The NHS is in the middle of its worst winter in a generation, with senior doctors warning that hospitals are facing intolerable pressures that are costing lives.”
The article adds that,
“The health service was already under pressure – the result of long-standing problems – but Covid, flu and now strike action by staff have all added to the sense of crisis this winter.”
Strike action by staff was not restricted to the early winter months, further strikes have occurred very recently. On 12th March, the BBC reported the then impending 3-day strike by junior doctors in an article entitled Why are doctors demanding the biggest pay rise?
“On Monday, thousands of junior doctors in England will start a 72-hour strike. They want a 35% pay rise. Yet doctors are among the highest paid in the public sector. So why do they have the biggest pay claim?”
A key concern will be that these strikes will cost lives.
A 13th March BBC article entitled I’ve never seen the NHS this bad – junior doctor refers to the conditions suffered by junior doctors that include workplace pressures and financial difficulties.
These conditions are not exclusive to junior doctors!
The point of these reports would seem to be to foster public sympathy and support for the junior doctors and deepen people’s concern for the future of the NHS.
The ‘official’ view of the pressures on the NHS is endorsed by a June 2022 opinion article entitled The steady crisis across the NHS published in the BMJ, which claims that the main issue is ‘chronic workforce shortages’ and states,
“The NHS has shown in the past that it can deliver rapid improvements to patient care when it has enough staff to tackle these challenges. If we want to break the cycle of consistently poor performance, the government needs a fully funded workforce plan for the whole health and social care system.”
The emphasis in these articles is clearly on the idea that doctors save lives and that they need better pay and working conditions, without which they would be unable to provide the proper level of care for their patients, as the 13th March article indicates,
“More pay and better working conditions would allow doctors to retain a work-life balance and would allow them to deliver the care they wanted to deliver, he said, adding taking industrial action was a “last resort” for doctors.”
The problem is that this is not an accurate view of the real problems and the inability of the NHS to provide adequate ‘healthcare’ to patients and enable them to be restored to health.
One of the alleged ‘problems’ that face the NHS, and every other ‘health service’ based on the practices of ‘modern medicine’, is expressed by the January BBC article, which states that,
“Advances in medicine over recent decades have meant people are living longer.
That is a success story. But it means the NHS, like every health service in the developed world, is having to cope with an ageing population.”
This is a misleading perspective – to put it mildly!
I must make it absolutely clear that I am not denying that there are some situations in which doctors absolutely do save lives – these situations mainly occur at the scene of accidents or emergencies or within the A&E (accident & emergency) department of hospitals. This is where the NHS provides an invaluable service.
However, can it really be claimed that the NHS and all other medical systems based on ‘modern medicine’ actually save lives in situations other than accidents and emergencies?
The evidence strongly suggests that this is not the case.
In response to a June 2000 article in the BMJ entitled Doctors’ strike in Israel may be good for health is a comment dated March 2001 with the intriguing title Doctor strikes, lowered mortality – Happens every time which includes the following,
“The 1960’s saw physicians in Canada go on strike and the mortality rate dropped.
Los Angeles physicians associated with a USC hospital went on strike in the 1970’s and the mortality rate dropped.
Physicians went on strike in South America (Columbia?) later that same decade and the mortality rate dropped.
Physicians have now gone on strike on 3 different occasions in Israel –in the 1950’s, again in the 1970’s or 80’s and now in the the year 2000. In all 3 occasions the mortality rate has dropped, on one or two occasions by 50%.”
In a December 2008 study article published on PubMed and entitled Doctors’ strikes and mortality: a review, the authors report their review of strikes around the world between 1976 and 2003 and state, with respect to the 7 studies they found that matched their criteria,
“All reported that mortality either stayed the same or decreased during, and in some cases, after the strike. None found that mortality increased during the weeks of the strikes compared to other time periods.”
One of the ‘reasons’ given is that elective surgeries were halted during the strikes. But this does not explain why mortality reduced – surely a lack of doctors ought to result in higher mortality!
For an explanation of why mortality decreases when doctors strike, I would remind readers of the phenomenon known as ‘iatrogenesis’ and recommend the July 2000 JAMA article by Dr Barbara Starfield MD entitled Is US Health Really the Best in the World? In her article, Dr Starfield shows that Americans are by no means the healthiest in the world, despite the huge costs of healthcare in that country. (The links to all articles can be found in the References at the foot of this article.)
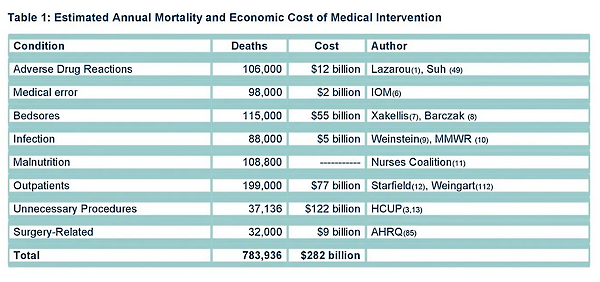
I would also recommend people read the Death by Medicine study by Gary Null et al. that includes the chart in the image below.
 The conclusion, which may be unpalatable to many people – although that does not make it untrue – is succinctly stated by the author of the March 2001 BMJ article,
The conclusion, which may be unpalatable to many people – although that does not make it untrue – is succinctly stated by the author of the March 2001 BMJ article,
“Conclusion? I’m sorry to say, but conventional, allopathic, (drug and surgery happy) physicians remain very, very dangerous to our health…”
The sad truth is that ‘modern medicine’ is not a ‘healthcare system’. Instead, as more people are discovering for themselves, it is a ‘sick-care’ system that merely manages symptoms but never truly allows people’s bodies to heal. The reason for this is because ‘modern medicine’ is based on a faulty paradigm and relies on our continuing ignorance of this fact to perpetuate that flawed system.
The empowering truth, by contrast, is that the human body is an amazing living organism that has the ability to self-heal – but implementing this understanding within our lives requires us to reclaim responsibility for our health and not outsource our healthcare to flawed systems that have no understanding of the body’s innate self-healing abilities.
Cover image credit: cromaconceptovisual

Truth Comes to Light highlights writers and video creators who ask the difficult questions while sharing their unique insights and visions.
Everything posted on this site is done in the spirit of conversation. Please do your own research and trust yourself when reading and giving consideration to anything that appears here or anywhere else.