Rabies: The “Virus” of Fear
Rabies: The “Virus” of Fear
by Mike Stone, ViroLIEgy
August 8, 2022
While walking down the darkened street late at night, have you ever had that gnawing fear as to whether or not the posse of raccoons rummaging through the trashcans nearby, staring at you with their beady yellow eyes, are ready and waiting for the right moment to pounce? Or have you ever had your fingertip accidentally pierced by the sharp fangs of a squirrel while feeding it walnuts and had to rush to the hospital on a nurses advice only to be told by the doctor that squirrels do not carry the “deadly virus?” Have you ever been bit in the very tender thin space of skin in between your thumb and index finger by a baby penguin while feeding it fish at the Omaha Zoo? Ok, the last one is obviously not related to rabies as the “virus” discriminates as to which animals it infects. Whether or not the squirrel can get or transmit rabies depends upon who you ask. In any case, these are all true experiences for me and yes, I have been bitten by numerous animals while feeding them. Like many, I have encountered the fear of being infected by a bite from a potentially rabid animal and that if I waited too long to receive treatment, it would be too late to stop the “virus” before it invades my cerebral cortex and causes me to turn into a crazed barking dog-man. Fortunately, not one of my comedically unfortunate puncture wounds left me to succumb to any disease. As I would later find out, my fears were in fact as irrational as the myths surrounding rabies which are built upon a foundation of fraud and pseudoscience.
Still, rabies seems to be one of the diseases that those who cling to the “virus” narrative love to bring up as if it is the Holy Grail of proof that “viruses” actually exist. Over the decades, the images of the mangy frothing dog snarling and ready to attack has been deeply ingrained into our subconscious through effective media fear-based propaganda.

The portrayal of angry diseased animals heightened peoples fear of anything wild and undomesticated and created in their minds the living walking embodiment of an invisible “virus” coming to infect the defenseless with a slobbery bite. The fear of aquiring the deadly disease was the perfect tool to use by Louis Pasteur in the late 1800’s to ensare people into the emerging germ theory narrative. All it takes is one bite for the sneaky “virus” to find its way into the bloodstream, attacking the brain and causing a painful death. It seems, upon first glance, to be an open and shut case. However, what you will find upon researching rabies is that the presented model of the rabid animal bite transferring an infectious “virus,” which in turn causes disease, is not an accurate portrayal whatsoever and was merely a frightening myth used to propagate the delusions of a madman looking to aquire fame, fortune, and prestige.
A few months ago, I looked at the unethical and fraudulent practices Louis Pasteur employed in the 1880’s in his attempt to prove a rabies pathogen exists and causes disease in order to sell his vaccines. Pasteur openly admitted to not being able to isolate any microorganism said to cause rabies but developed his vaccine against the invisible pathogen anyways. This is also openly admitted as well by the Institut Pasteur:
“Louis Pasteur’s initial efforts to isolate the rabies virus proved unsuccessful as the virus remained invisible. Viruses could not be seen due to the poor resolution of the microscopes used. The virus was not seen until almost a century later, in 1962, with the advent of electron microscopy.
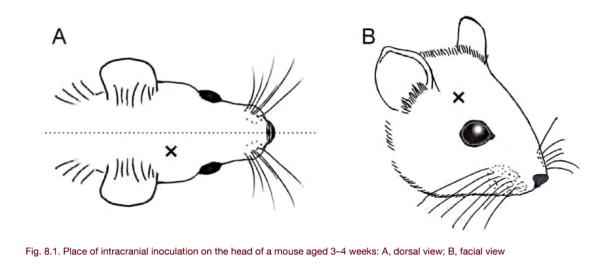
But as rabies is a disease of the nervous system, together with Emile Roux, Louis Pasteur then had the idea of inoculating part of a rabid dog’s brain directly into another dog’s brain. The inoculated dog subsequently died.”
https://www.pasteur.fr/en/institut-pasteur/history/troisieme-epoque-1877-1887
Thus, Pasteur never worked with any purified and isolated “virus” and did what virologists still do today, which is assume an invisible entity is floating freely in the unpurified solutions of diseased animals which are then inoculated into healthy animals in attempts to cause disease and prove pathogenicity. Interestingly, as stated in the 1930 paper below, Pasteur would fail many times in his attempts to infect animals with saliva from animals claimed to be rabid, the very fluids the “virus” is supposed to reside in. Even if deemed successful, the symptoms would not appear for months, which was unheard of for any pathogen. Thus, he sought other means of infecting animals by way of injecting dogs directly in the brain with the emulsified cranial goo from animals claimed to be rabid. Once the healthy animal died from the toxic brain injection, this was considered a success:
Pasteur’s Work with Rabies
“Inoculation with saliva was found to be a method which did not always produce rabies and symptoms did not declare themselves for months. The theory that the disease virus attacks the nerve centers had already been set forth by Dr. Dubous of Paris. Pasteur accordingly inoculated a number of animals subcutaneously with some of the brain substance from other animals which had died of rabies. Most of those inoculated developed rabies, but not all.
Pasteur then conceived the idea of introducing into the brain of experimental animals some of the nerve tissue from an animal which had died of rabies. This experiment was based on the principle of providing the causal organisms with the nutritive medium best suited to their requirements. Pasteur, obliged to sacrifice so many animals, had a real dislike for vivisection; if the animal cried out a little he was full of pity. The idea of perforating the skull of the dog was repulsive to him, he wanted it done but dreaded seeing it done. So it was done one day when he was away. The next day when he was told of the intra-cranial inoculation he was moved to pity for the poor dog.”
https://doi.org/10.2307/3410286
While the exact make-up of the inoculations remain a mystery due to Pasteur’s secretive nature, the vaccine’s he utilized contained a neurotropic agent which was known to cause the exact same neurological conditions as seen in rabid animals. While injecting anything into the brain would potentially cause neurological damage and death, it is not far fetched to believe Pasteur used the same neurotropic agents in his experimental inoculations to prove pathogenicity, especially as they were said to consist of emulsified brain and nervous tissue. This created an issue in determining whether it was the invisible “virus” or the injections themselves which caused neurological damage and/or death. However, it has been admitted that the vaccines themselves led to the majority of neurological conditions rather than “wild” rabies cases as this was considered a rare occurrence in nature. This is just another in a long history of cases where the vaccine created the disease it was supposed to be preventing.
Fortunately, we can learn a lot of interesting tidbits about rabies (or the lack thereof) from the work of Gerald Geison, a leading Louis Pasteur researcher and historian who was privy to his private notebooks. In a 1978 essay he wrote on the ethics of rabies vaccination, Geison pointed out some of the pecularities of rabies such as the fact that it has always been considered a rare disease in man as well as the fact that rabies can not be transmitted from person-to-person. He also noted that, as a pathogenic disease, rabies has an unusually long incubation period. While it is said to usually last 6 to 8 weeks, Geison claimed that it can actually last for a year or more. In fact, there have been reported cases with a rabies incubation period from 6 years all the way on up to 25 years. If that wasn’t outlandish enough to make one question the validity of what we are told of the disease, Geison stated that there was a high degree of uncertainty regarding the correlation between animal bites and rabies symptoms as well as the threat of death from being bitten by a clearly rabid animal:
Pasteur’s Work on Rabies: Reexamining the Ethical Issues
“Rabies has always been rare in man. It probably never claimed more than a hundred victims in any year in France, and Fiench estimates for the years immediately preceding Pasteur’s famous work indicate an annual mortality of considerably less than fifty. In addition, rabies is not an infectious disease in the usual sense; it is not transmitted from man to man. Because of these two features, general or compulsory vaccination has never seemed appropriate with respect to rabies.
“An even more peculiar feature of rabies is its long incubation period in the absence of detectable symptoms. No other lethal disease of rapid clinical course even approaches rabies for length of incubation-usually six to eight weeks, but sometimes a year or more.
“Unfortunately for Pasteur and his successors, there is a very high degree of uncertainty in the correlation between animal bites and the subsequent appearance of rabies-even when the biting animal is certifiably rabid. While the mortality of clinical rabies is virtually 100 percent, the threat of death from the bite of a rabid animal is vastly less. The risk depends on several factors, including the species of attacking animal (wolf and cat bites, for example, pose a much higher risk than dog bites), the location and depth of the bites, and the application or timing of cauterization. Depending on these and other circumstances, estimates of the risk of contracting rabies from the bites of animals known to be rabid range from as high as 80 percent to as low as 0.5 percent. It is perhaps futile to try to settle upon a meaningful “average” figure within this range, but Pasteur himself estimated that 16 percent of those bitten by rabid dogs would eventually die of rabies unless they submitted to his new treatment.”
In his 1995 book The Private Science of Louis Pasteur, Geison pointed out that, according to the English Commission on Rabies, there was also much uncertainty in the rabies statistics. They had suspected that at least one man had died not from rabies but from Pasteur’s vaccine instead and they actually favored animal regulations over Pasteur’s vaccination approach:
“But the English commission also drew attention to the uncertainty of all statistics on rabies, citing the difficulty of establishing that the attacking animal had in fact been rabid as well as the variable effects of the location and depth of bites, of differences in the lethality of rabid animal bites in different species and races, and of the possible prophylactic effects of cauterization or other treatments applied to bitten victims before they submitted to Pasteur’s treatment. The commission also suspected that at least one man may have died as a direct result of the Pastorian injections, and in the end it favored strict regulations on potentially rabid animals (muzzling and quarantine) over Pasteur’s more drastic remedy.”
We also find out from Geison that, in great contrast to what we are told about rabies, the great majority of rabies victims could forgo any treatment and never have any ill effects whatsoever:
“In short, the great majority of the victims of rabid animal bites could forgo Pasteur’s treatment without experiencing any untoward consequences in the future. And they had to decide whether or not to submit to the treatment at a point when they had no symptoms of the disease. For the efficacy and very possibility of Pasteur’s vaccine depended on the peculiarly long incubation period that separates the infective bites of a rabid animal from the outbreak of symptoms.”
Geison even spotlighted what was known as “false rabies,” which were cases of the exact same symptoms of disease associated with rabies that occured despite a complete lack of the victim being bitten by a rabid animal. These symptoms were said to be either induced solely based on fear alone or by alcoholism. In other words, just the mere thought of rabies could create an intense enough reaction inducing the same disease, thus no invisible microscopic pathogen is necessary. Pasteur actually emphasized these cases in defense of his vaccine as there was a growing chorus of criticism that his vaccine did not protect the victims and in fact induced the symptoms of rabies which lead to their deaths. Pasteur therefore had a vested interest in showing that these same symptoms could occur outside of animal bites and vaccination:
“Pasteur himself later pointed out some of the uncertainties surrounding the diagnosis of rabies. Two years after I’affair Girard, for example, he spoke to the Academie des sciences about several cases of “false rabies.” Relying on the authority of one Dr Trousseau, Pasteur cited two cases in which symptoms of the disease had been induced solely by fear. In one case, a man suddenly displayed several of the classic features of rabies—including throat spasms, chest pain, extreme anxiety, and other nervous symptoms—merely because the disease had become the subject of a lunchtime conversation. And this man had never even confronted a rabid animal. Presumably more common was the second case, that of a magistrate whose hand had long before been licked by a dog later suspected of rabies. Upon learning that several animals bitten by this dog had died of rabies, the magistrate became extremely agitated, even delirious, and displayed a horror of water. His symptoms disappeared ten days later, when his physician persuaded him that he would already be dead had he been afflicted with true rabies.”
In this same address, Pasteur commented upon a recently published case history of “false rabies.” Partly because it includes an arresting account of the classic symptoms of rabies, his commentary deserves quoting at length. As recorded in the Comptes rendus of the Academie des sciences for 17 October 1887, Pasteur spoke as follows:
The patient to whom Mesnet refers in his brochure was an alcoholic who, having seen some sort of deposit m his glass during lunch, was seized by a feeling of horror toward the liquid and by a constriction of the throat, followed by headache and by lameness and fatigue in all his limbs. He spent Sunday in this state.
During that night and during the day on Monday and Tuesday, no sleep, a fit of suffocation, throat spasms, and a horror of liquids, which he pushed aside in his glass. His countenance expressed disquiet. His eyes were fixed, glazed, the pupils greatly dilated. His speech was brief, jerky, rapid. He had difficulty breathing. When he was offered a glass of water, he pushed it aside with terror, and suffered fits of suffocation and of constriction of the throat. Bright objects and light were particularly disagreeable to him. He was painfully affected when the air was agitated in front of his face. He died Wednesday night after having suffered from a violent delirium, with extreme agitation, howls and cries, extremely abundant salivation, spitting, biting his bedsheets, and trying also to bite the person taking care of him. In short, this man displayed all the features of furious rabies [I’hydrophobie funeuse]. But he did not die of rabies. He had never been bitten and on several occasions, at long intervals, had already displayed symptoms analogous to false rabies. This man was an alcoholic and belonged, moreover, to a family m which one member had died of insanity [alienation mentale].
By October 1887, when he gave this address, Pasteur had a vested interest in emphasizing the difficulty of diagnosing rabies. For he was then defending himself against allegations that his rabies vaccine not only sometimes failed to protect those who submitted to it, but in some cases was itself the cause of rabies and therefore death. A few hostile critics were insisting that some people died of rabies not only despite Pasteur’s vaccine but because of it, and they tried to make Pasteur and his treatment responsible for the death of anyone who displayed any symptoms of nervous disease. In defense of his vaccine, Pasteur now emphasized the extent to which symptoms like those of rabies could appear in patients who did not have the disease. He therefore insisted that a diagnosis of rabies could only be established with confidence by experiments in which tissue from the victim’s brain was transmitted to animals susceptible to the disease.”
https://www.jstor.org/stable/j.ctt7zv2b1
There is good reason for the high degree of uncertainty over the correlation between animal bites and the development of symptoms, the actual rabies statistics, as well as the ability to accurately diagnose the disease. For starters, there are many other conditions that can cause the exact same symptoms as rabies in both animals and in humans. In animals, canine distemper, encephalitis, and poisoning are a few of the conditions which can mimic rabies. In humans, this includes polio, being drunk and/or intoxicated on certain drugs, having Guillain–Barré syndrome, and as stated previously, encephalitis derived from the toxic vaccine itself.
It has been stated that it is common not to even find bite marks in cases of rabies and often, the person has had no idea that they were ever bitten to begin with. One source stated that fewer than one third of human rabies victims show evidence of bite wounds. With the vast range of conditions that mimic rabies and the lack of bite marks, it’s safe to question the existence of a specific disease known as rabies. It would be logical to conclude that rabies is nothing but the same set of symptoms that has been given a different label numerous times.
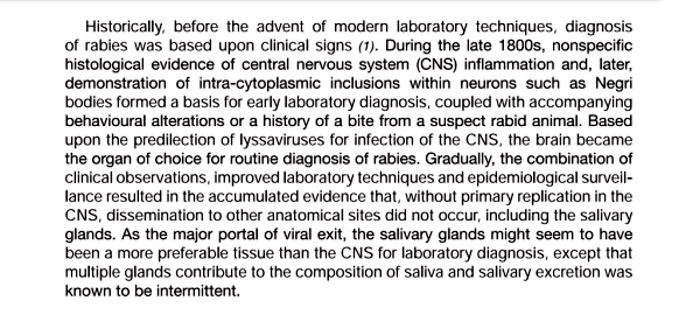
This uncertainty in rabies cases and statistics boils down to the inability to accurately diagnose a rabies case. For much of the 1800s to the mid 1900s, rabies was diagnosed upon clinical symptoms which, as previously stated, were not specific to the disease. It is also noted in the WHO’s rabies laboratory manual that the histological diagnosis for rabies, which began in the late 1800’s, was also non-specific:
When factoring in the non-specificity in diagnosis, the uncertainty in the correlation between animal bites and disease symptoms, and the vast majority of victims never needing any treatment whatsoever, it leads one to conclude that the rabies myth is vastly overstated. It is fictitious fear propaganda rather than facts based in reality. We can break this deception down even further by looking at how rabies is diagnosed in the present versus how it was in the past. According to the CDC:
Diagnosis in animals
“A diagnosis of rabies can be made after detection of rabies virus from any part of the affected brain, but in order to rule out rabies, the test must include tissue from at least two locations in the brain, preferably the brain stem and cerebellum.
The test requires that the animal be euthanized. The test itself takes about 2 hours, but it takes time to remove the brain samples from an animal suspected of having rabies and to ship these samples to a state public health or veterinary diagnostic laboratory for diagnosis.”
https://www.cdc.gov/rabies/diagnosis/animals-humans.html
In order to diagnose rabies, the animal must be killed and sections must be taken from the brain in order to try and detect the “virus.” We already have a few problems here as no “virus” was ever purified and isolated in order to determine how to detect it. There is also an issue with attempting to determine anything from dead tissue as the tissue, once removed, immediately starts to change through decomposition. Biologist Harold Hillman often pointed out the faults in trying to establish credible information about what occurs inside living beings from the study of dead tissues:
“Killing an animal changes its biochemistry grossly. For example, its blood carbon dioxide, phosphate, lactate, and potassium ion concentrations, rise, while its oxygen, sodium ion, adenosine triphosphate, phosphocreatine, concentrations go down. These changes affect much of the tissue metabolism. It is hoped and normally assumed that they will reverse during incubation. There is no realistic way of testing this, since the volume and chemistry of the tissue changes during incubation. In this circumstance, it is worth asking whether cell biologists should use tissues in vitro at all. Perhaps, they should confine their experiments to working on intact animals and human beings, tissue cultures, unicellular organisms and plants.”
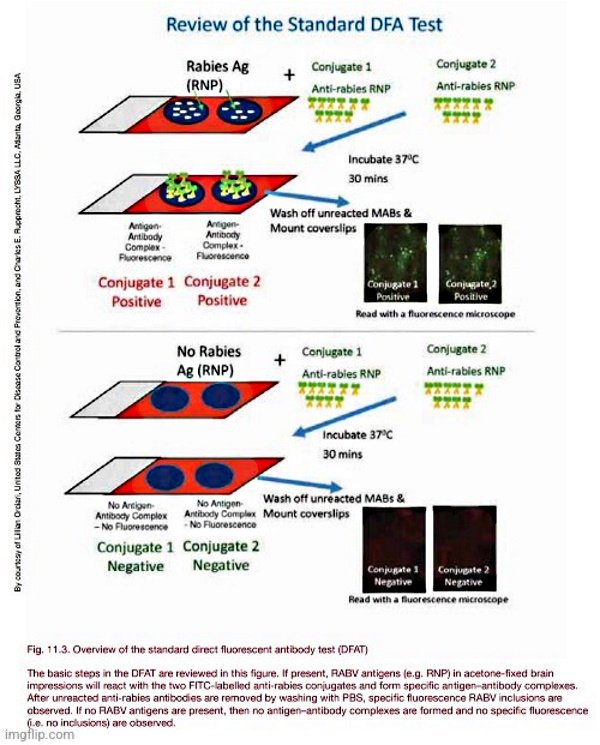
The current “gold standard” used to study the dead brain tissue for the diagnosis of rabies is known as the direct fluorescent antibody test. As the name implies, the test looks to detect rabies antigens on the brain by using antibodies said to be specific to the rabies “virus:”
Direct Fluorescent Antibody Test
“The dFA test is based on the observation that animals infected by rabies virus have rabies virus proteins (antigen) present in their tissues. Because rabies is present in nervous tissue (and not blood like many other viruses), the ideal tissue to test for rabies antigen is brain. The most important part of a dFA test is flouresecently-labeled anti-rabies antibody. When labeled antibody is incubated with rabies-suspect brain tissue, it will bind to rabies antigen. Unbound antibody can be washed away and areas where antigen is present can be visualized as fluorescent-apple-green areas using a fluorescence microscope. If rabies virus is absent there will be no staining.”
https://www.cdc.gov/rabies/diagnosis/direct_fluorescent_antibody.html
According to the CDC, in the 50 years that the dFA test has been used to detect rabies, it has not failed to present reliable and accurate results. This indirect method is somehow said to be more sensitive and specific than actually “isolating” the “virus,” thus the “gold standard” label. It is also stated by the CDC that the saliva of an infected animal contains millions of “virions,” making the lack of any purified and isolated “virus” and the reliance on indirect antibody testing all the more glaring of an issue:
Accuracy of the Tests
“During the 50 years the direct fluorescent antibody (DFA) test has been used in the United States, there has been no indication it has failed to provide accurate clinical information on the rabies status of an animal for the purposes of treating an exposed person.
Because of its high sensitivity and specificity, in comparison to virus isolation methods, the DFA test is the “gold standard” diagnostic method for rabies and has been rigorously evaluated by international, national, and state health laboratories. The DFA test is currently the only recommended diagnostic method for routine rabies determination in animals in the United States.
During clinical disease, millions of viral particles may be found intermittently in the saliva. In theory, only a single rabies particle or virion is required to result in a productive infection.”
https://www.cdc.gov/rabies/diagnosis/accuracy.html
Returning to the WHO’s rabies manual, it shows us exactly how the dFA is used and how the diagnosis is determined based on the interpretation of the person reading the results. The interpreter uses an antigen fluorescence intensity and distribution scale from +4 on down to +1 to determine one of four conclusions: positive, negative, unsatisfactory, or inconclusive. Obviously, the subjective bias of the interpreter plays no role in the accuracy of the determination as humans rarely make interpretive errors, correct?:
From the WHO’s Laboratory Techniques in Rabies:
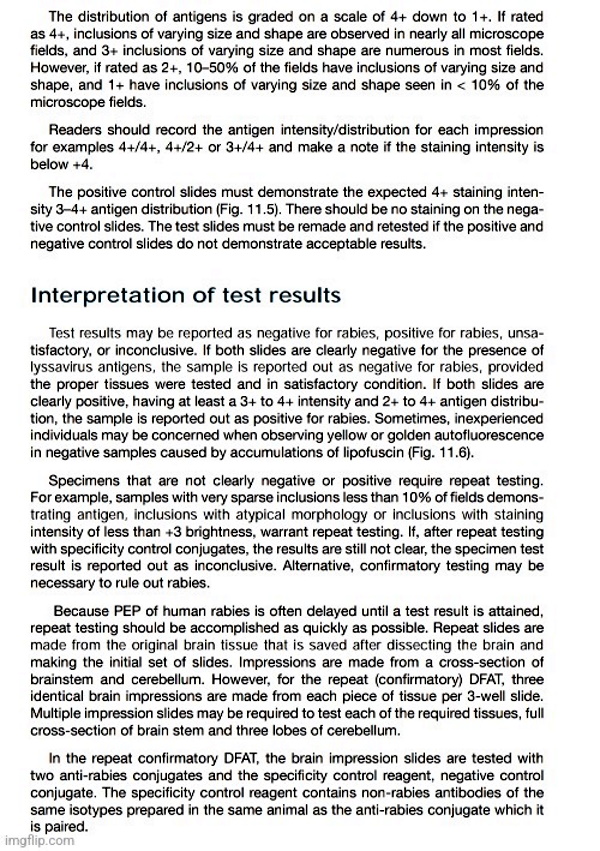
https://apps.who.int/iris/bitstream/handle/10665/310836/9789241515153-eng.pdf
In fact, there are many drawbacks to using the dFA as the “gold standard” test for rabies diagnosis beyond the aforementioned use of dead tissues. For starters, due to the lack of ever properly purifying and isolating the rabies “virus” directly from the saliva said to contain millions of “virions,” any antibody result is utterly meaningless as there is no “virus” to determine a specific reaction with. We also have this same purification/isolaton problem with antibodies as these entities have also never been taken and separated directly from the fluids of a host in order to be studied independently. There is also the issue that the theoretical antibodies themselves are entirely non-specific and are regularly said to bind to proteins that are not the intended target. Thus, we once again run into the problem where one fictional entity (the rabies “virus”) is said to be detected by another fictional entity (the antibody). It is very telling that the CDC believes that the interpretive results from this indirect circular test is more accurate than actually finding and “isolating” the supposed “virus.”
Thus, we must ask ourselves if these dFA tests really are as accurate as stated by the CDC. If we do so, we find out that this is most definitely not the case according to these next three sources. This first snippet comes from a study done on bacteria which points out the obvious fault of the subjective interpretation of the dFA test results which leads to poor sensitivity and a widely varying specificity, contrary to the claims made by the CDC:
“Direct fluorescent-antibody testing (DFA) provides a much more rapid result but also has the disadvantage of poor sensitivity, and its specificity varies widely due to the subjective interpretation of test results.”
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC85400/
This second study also points out the flaws of the subjective interpretation of the test results as well as the need for expensive equipment and quality-controlled reagents, the varied parameters utilized for succesful results and the issues relating to the incubation times and temperatures, as well as the necessity of having well-trained personnel running and interpreting the results:
“However, DFA has several drawbacks such as the need for an expensive fluorescent microscope, well-trained personnel, and quality controlled reagents (antibodies, conjugates), and varied parameters used during microscopy, and incubation times and temperatures, not to mention the subjectivity in interpretation of the test results [27,28,29,30]. In addition, acetone used as fixative in DFA does not completely inactivate the virus, as demonstrated by the infectivity of acetone-fixed tissue for neuroblastoma cells [31], posing a potential biohazard to laboratory personnel. Indeed, complete inactivation of cell culture-derived rabies virus appears to require >30% acetone [32].”
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5876580/
And finally, from this 2017 study published in PLOS Neglected Tropical Diseases, we can once again see the problems with subjective interpretation of dFA test results in action. The study utilized 23 independent laboratories to aid in identifying “differences in the laboratory protocols that could explain discrepant laboratory results and provide baseline knowledge for regional standardization of protocols.” The labs were each sent 20 samples which included 17 test samples and 3 controls. The positive tissues contained major rabies “virus” variants that were circulating in the Americas while the negative samples consisted of tissues demonstrating complete absence of rabies “virus” antigen and artifacts. Each lab was asked to test the samples using their own standard protocols and to record their results (positivity, intensity, and distribution of the fluorescence staining) as well as the microscopic condition and impression quality of the tissues (Good, Acceptable, or Deficient) as evaluated by the laboratory operator. The results from this 2017 study indicated that there are substantial differences in the overall dFA results and test interpretation as the “level of concordance between the 23 participating laboratories and the CDC panel showed large variability.” Only two laboratories had 100% concordance, while 91% of the labs had at least one discordant sample, with a total of 26 false positive and 61 false negative results among all laboratories:
An inter- laboratory proficiency testing exercise for rabies diagnosis in Latin America and the Caribbean
“Our results indicate that although all laboratories can perform the direct fluorescent antibody test, there are substantial differences in the overall results and test interpretation. This study identified important gaps in standardization and/or harmonization between laboratories which could be overcome and corrected with appropriate DFA protocols standardized across the LAC, including its broad distribution and proper training.”
“Conclusive rabies diagnosis can only be achieved by appropriate laboratory testing. Clinical and epidemiological diagnosis is challenging and leads to under-reporting [1, 2, 3]. The Direct Fluorescent Antibody test (DFA) for detection of rabies virus antigen remains as the gold standard test for laboratory diagnosis of rabies in post-mortem brain tissues [3].”
“The agreement between the laboratory results and those of the CDC, as measured by the sensitivity, specificity, concordance and kappa values are shown in Table 2. Two laboratories correctly identified all samples tested (sensitivity and specificity of 1.0). However, 30% (7/23) of all laboratories reported at least one false positive and 83% (19/23) of all laboratories reported at least one false negative sample. The average sensitivity was 76% with a range of 40% to 100%. The average specificity was 88% with a range of 22% to 100%. While a majority of the laboratories had low false positive rates, there were considerable differences in the sensitivity (Fig 1). The mean concordance was 81% with a range of 50% to 100% and the mean kappa score was 0.56 with a range of 0.02 to 1.00.”
“The level of concordance between the 23 participating laboratories and the CDC panel showed large variability. Two laboratories had 100% concordance, while 91% of the labs had at least one discordant sample, with a total of 26 false positive and 61 false negative results among all laboratories.”
“The type of conjugate may also affect the sensitivity of the DFA test (monoclonal cocktail versus polyclonal, in-house made versus commercial). For the current exercise, laboratories used commercial (65%) or in-house (35%) conjugates. A study of 12 rabies reference laboratories in Europe demonstrated that the variability of conjugates could potentially lead to discordant results and influence assay sensitivity [19].”
https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0005427
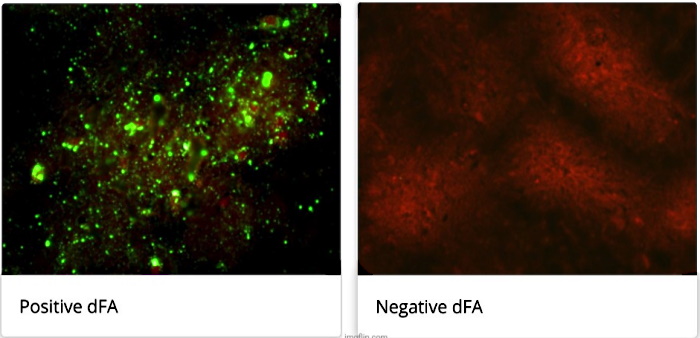
A bunch of glowing green dots means…absolutely nothing.In answer to the claim by the CDC that “during the 50 years the direct fluorescent antibody (DFA) test has been used in the United States, there has been no indication it has failed to provide accurate clinical information on the rabies status of an animal for the purposes of treating an exposed person,” we can safely conclude that this is obviously a false statement. The dFA test has been shown to have low sensitivity and a widely varying specificity as well as major issues relating to the subjective interpretation of the results based upon the person doing the interpreting. The 23 labs participating in the 2017 study had large variability in concordance with the CDC’s own panel. Anyone looking at this indirect test with a shred of intellectual honesty can easily see that the CDC’s “golden standard” rabies test does not look so golden anymore.
While the dFA test is the “go to” diagnostic measure in modern times, there are other methods available which can be used in an attempt to claim an animal is infected with the rabies “virus.” One of these is the “isolation” of the “virus” in tissue and cell cultures, which used to be the “gold standard” method for proving a “virus” exists and is infectious. Oddly enough, the CDC stated that the supposed “isolation” of the rabies “virus” is not as sensitive nor as specific as the dFA test. How could this possibly be the case?
For one thing, it is admitted that the rabies “virus” does not actually produce the desired cytopathogenic effect (CPE) when cultured:
Detection of rabies virus replication: inoculation tests
“The other group of available techniques aim at detecting the replication of the virus on living substrates, e.g. cells. Virus isolation may be necessary to confirm inconclusive results in FAT/dRIT and for characterization of the virus strain. In neuroblastoma cells, rabies virus grows generally without cytopathic effect; once again it is necessary to use FAT to confirm the presence of rabies virus. After intracranial application, rabies induces clinical signs in mice that are relatively typical but have to be confirmed by FAT. Since cell culture is as sensitive as the mouse inoculation test, units should be established in laboratories to replace mouse inoculation tests as it avoids the use of life animals, is less expensive and gives more rapid results.”
https://www.who-rabies-bulletin.org/site-page/diagnosis-rabies
Why is this important to note? The cytopathogenic effect (CPE) is the structural and morphological changes to the cell that are claimed to be caused by the “virus” as it enters the cell, breaking it apart as the “virus” creates more copies of itself. This effect is supposed to tell the researchers that the “virus” is present within the culture. According to their stories, without this effect, it should be a clear indicator that the host was not infected by the “virus.” However, virology loves to bend their own rules and in a clear cut case of having their cake and eating it too, virologists claim that certain “viruses” do not cause CPE in their natural host cells. They state that there are different levels of CPE based on the cell type used:
- Not permissive cell – virus cannot infect
- Permissive cell – virus can replicate, but does not cause obvious CPE
- Highly permissive cell – virus replicates and induces an obvious CPE
https://cytosmart.com/resources/virus-induced-cytopathic-effect
Anyone looking at this logically can see that “Not permissive” and “Permissive” cells are the exact same thing. Neither of these cells produce CPE when “infected” by the “virus.” However, virologists will resort to other indirect measures in order to claim the “virus” is present in spite of the lack of any CPE observed. In the case of rabies, the dFA test is used to confirm if a “virus” is present in a culture. However, if the dFA test is considered inconclusive, the cell culture is used to confirm the dFA result. A bit circular there, don’t you think? Another confirmation is done by injecting the toxic CPE-less cell culture soup into the brain of a mouse and seeing if symptoms occur. If so, the mouse is killed and the newly damaged brain is taken and tested by dFA for confirmation. Seeing the problem yet?
If neither dFA and/or cell culturing is enough satisfactory indirect evidence to claim the existence of the rabies “virus,” one can turn to the old ways of histopathology to try and build a circumstantial case against the invisible entity. Along with attempting to diagnose someone based on clinical symptoms, which thanks to Louis Pasteur and “false rabies” we know is inaccurate due to the non-specificity of the symptoms, histopathology was the main method utilized for decades for determining if an animal was in fact rabid. This consisted of staining the brain tissues with chemicals such as hematoxylin and eosin and looking for patterns of encephalopathy as well as the presence of what are called Negri bodies. Negri bodies are round or oval inclusions within the cytoplasm of nerve cells of animals which were discovered by Dr. Adelchi Negri in 1903. At the time, he claimed that these inclusions were the etiologic agent of rabies. While the rest of the virology community disagreed with Dr. Negri, his discovery was considered a tell-tale sign of rabies infection in the brain and finding these inclusions served as the basis for a rabies diagnosis for over 60 years. However, there is rather big problem for these histopathological examinations. Signs of encephalitis and finding Negri bodies are both entirely non-specific and are seen in cases that have absolutely nothing to do with rabies. In fact, Negri bodies are said to only be found in half of the cases of rabies:
Histologic examination, General histopathology
“Histologic examination of biopsy or autopsy tissues is occasionally useful in diagnosing unsuspected cases of rabies that have not been tested by routine methods. When brain tissue from rabies virus-infected animals are stained with a histologic stain, such as hematoxylin and eosin, evidence of encephalomyelitis may be recognized by a trained microscopist. This method is nonspecific and not considered diagnostic for rabies.
Before current diagnostic methods were available, rabies diagnosis was made using this method and the clinical case history. In fact, most of the significant histopathologic features (changes in tissue caused by disease) of rabies infection were described in the last quarter of the 19th century. After Louis Pasteur’s successful experiments with rabies vaccination, scientists were motivated to identify the pathologic lesions of rabies virus.
Histopathologic evidence of rabies encephalomyelitis (inflammation) in brain tissue and meninges includes the following:
- Mononuclear infiltration
- Perivascular cuffing of lymphocytes or polymorphonuclear cells
- Lymphocytic foci
- Babes nodules consisting of glial cells
- Negri bodies
Negri bodies
In 1903, most of the histopathologic signs of rabies were recognized, but rabies inclusions had not yet been detected. At this time, Dr. Adelchi Negri reported the identification of what he believed to be the etiologic agent of rabies, the Negri body. In his report, he described Negri bodies as round or oval inclusions within the cytoplasm of nerve cells of animals infected with rabies. Negri bodies may vary in size from 0.25 to 27 µm. They are found most frequently in the pyramidal cells of Ammon’s horn, and the Purkinje cells of the cerebellum.
They are also found in the cells of the medulla and various other ganglia. Negri bodies can also be found in the neurons of the salivary glands, tongue, or other organs. Staining with Mann’s, giemsa, or Sellers stains can permit differentiation of rabies inclusions from other intracellular inclusions. With these stains, Negri bodies appear magenta in color and have small (0.2 µm to 0.5 µm), dark-blue interior basophilic granules.
The presence of Negri bodies is variable. Histologic staining for Negri bodies is neither as sensitive nor as specific as other tests. Some experimentally-infected cases of rabies display Negri bodies in brain tissue; others do not. Histologic examination of tissues from clinically rabid animals show Negri bodies in about 50% of the samples; in contrast, the dFA test shows rabies antigen in nearly 100% of the samples. In other cases, non-rabid tissues have shown inclusions indistinquishable from Negri bodies. Because of these problems, the presence of Negri bodies should not be considered diagnostic for rabies.”
https://www.geosalud.com/pets/rabies_diagnosis.html
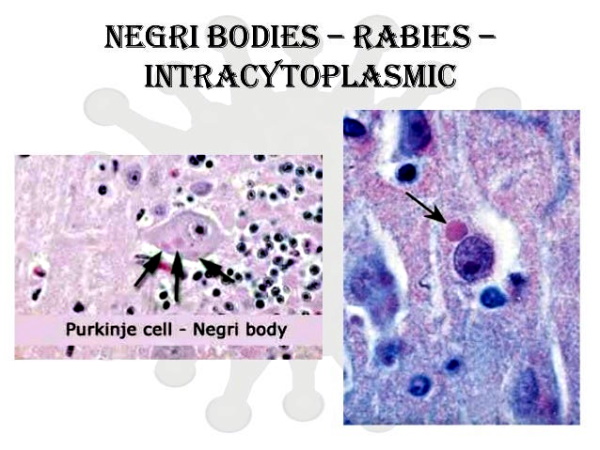
As the Negri bodies played such a substantial role in determining the diagnosis of rabies and building the case statistics used to sell the public on a “virus” in need of vaccination and eradication, let’s look at two more studies to find out a bit more about these non-specific diagnostic blobs. In 1942, it was already well known that the Negri bodies were not specific to rabies and could be mistaken for other inclusion bodies seen in the tissues upon examination. This is a rather big deal as the mass vaccination of dogs didn’t start for another 5 years in 1947. So we can already see that the main method used for diagnosis was faulty which casts doubt on any rabies statistics generated up to that time using this method. The authors go on to admit that there were deficiencies in the method used for examining these inclusions. It is stated that every experienced microscopist encountered difficulty in deciding whether or not the bodies observed were in fact Negri bodies or whether they were instead normal or possibly distorted cytoplasmic structures. In the study of 84 mice said to be given rabies by way of injection, Negri bodies were only found in the hippocampus 8 times as well as only 4 times in the cerebral cortex. The authors concluded that there are many rabies cases without Negri bodies present upon examination and that there are various structures which resemble Negri bodies commonly found in normal animals:
Problems in the Laboratory Diagnosis of Rabies*
“THE diagnosis of rabies in the laboratory is based entirely upon the microscopic demonstration of Negri bodies and upon animal inoculation. The demonstration of Negri bodies is the method of choice since the diagnosis can be thus made in a few minutes or hours. When the technic employed demonstrates typical bodies the result is highly convincing and satisfying. However, negative and doubtful results leave much to be desired, and animal inoculation must be resorted to. The difficulties in demonstrating Negri bodies arise from two sources of error which can be enumerated as inability to differentiate them from other inclusion bodies and cell structures, and inherent deficiencies in the methods of examination.”
“However, every experienced microscopist has encountered the difficulty of deciding whether the bodies observed in some preparations are Negri bodies or cytoplasmic structures normal to the cell or if not normal at least only distorted cellular structures. Goodpasture refers to the variation in size of Negri bodies and speaks of being able to demonstrate the smallest forms. When small bodies are associated with large ones, which show the typical inner structure, no confusion is encountered. When, however, only forms so small occur that the demonstration of the “Innenkorper” is doubtful, the diagnosis is doubtful. The brain of cats, particularly, offers difficulty because of the pink staining granular material in the cells and also because the Negri bodies in the pyramidal and Purkinji cells of this animal are often very small. The failure of the microscopic diagnosis of rabies as proved by mouse inoculation is shown in Table 1.”
“Above we have mentioned the occasional occurrence of what appear to be “lyssa bodies” or small Negri bodies in the brain of some animals which did not produce rabies when injected into mice. These bodies are found most frequently in the cerebrum and medulla. Since in the study of 84 cases of rabies proved by mouse inoculation we found Negri bodies only in the hippocampus 8 times and only in the cerebral cortex 4 times (Table 2), the finding of eosinophilic bodies in any portion of a brain from an animal suspected of having had rabies creates a doubt as to the diagnosis.”
“From these results it appears that by microscopic examination of sections and in some smears we are able to demonstrate eosinophilic bodies resembling “lyssa bodies” and atypical Negri bodies which are not associated in the brain with rabies virus. Also the results show that brain specimens in which the microscopic examination leaves the diagnosis in doubt contain rabies. The bodies that cause this confusion in the microscopic diagnosis of rabies are similar to ones found in certain parts of the brain of normal cattle and other animals and to atypical or small Negri bodies.”
doi: 10.2105/ajph.32.2.171.
While the 1942 study should have been the end of the Negri body as a diagnostic indicator of rabies, this method carried on being used over the decades. In 1975, another study emerged casting doubts on the dogma surrounding these long-held markers of the rabies disease. It’s stated that there was a universal acceptance of the Negri body as a specific indicator of rabies and that due to this widely-endorsed dogma, every time a Negri body was seen, a rabies diagnosis was made irrespective of the circumstances regarding the case.
However, in this study, a case was reported of a person who was considered rabies free by way of dFA and electron microscopy but Negri bodies were still found upon examination. This finding was inconsistent with the idea of the specificity of these bodies to rabies. The author pointed out many flaws with the use of Negri bodies as a diagnostic tool as outside of finding them upon examination, rabies is non-specific and mimics other diseases such as smallpox. It is stated that rabies encephalitis does not have any pathognomonic clinical or pathologic features distinguishing it from other diseases. The absence of Negri bodies in a substantial number of fatal cases of rabies, the lack of any inflammatory response, the absence of any history of animal contact in more than 30% of fatal cases, and the lack of specific behavioral symptoms of rabies in animals led the author to the conclusion that any association between this diagnostic method and the rabies disease is unwarranted. Thus, it is easy to see that any and all rabies case statistics based upon the clinical diagnosis and findings of Negri bodies should be thrown out:
Is the Negri Body Specific for Rabies?
“Of all viral diseases affecting the nervous systems of humans and animals, rabies seems to be the only one in which light microscopy alone can provide a definitive etiologic diagnosis. This is based on the universally accepted conviction on the specificity of the Negri body for rabies. Thus, the presence of a Negri body in the brain of a patient who did not have rabies is a matter that deserves attention.”
“Neuropathologically, the exclusion of rabies in the present case is based on the negative immunofluorescent
study results for rabies and the absence of the rabies virus within the Negri bodies (light microscope) as demonstrated by electron microscopy. Such an observation, of course, is inconsistent with the specificity of the Negri body in signifying the presence of rabies. Therefore, it is reasonable to ask: What are the other inclusion bodies that occur in sites other than the nervous system that are morphologically similar to Negri body?”“The result of a universally accepted dogma such as this is obvious; in every instance in which a “Negri body” has been seen, a diagnosis of rabies was made irrespective of the circumstances.
To delineate some of the related aspects of the problem the following points deserve etnphasis:
-
- Except for the occurrence of the Negri body, rabies encephalitis does not have any pathognomonic clinical or pathologic features. Variola-vaccinia virus, for example, can produce the same clinical pictures. The cutaneous manifestations can be sufficiently scanty to be missed on the physical examination, or they can be absent altogether (variole sans eruptione). There is remarkable variability in the intensity of cellular inflammatory response in rabies encephalitis. This, to some extent, may reflect the vigor with which these reactions are searched for, since the diagnostic efforts in the past have been mainly directed to the “specific” finding of the Negri body. The absence of Negri bodies in a substantial number of fatal cases of rabies and the remarkable lack of inflammatory response in some instances of the disease signify the importance of obtaining a careful history. A definitive etiologic diagnosis of rabies, however, requires obtaining positive results with immunofluorescent or electron microscopical methods or both. The former method maps the occurrence of rabies viral antigen in any morphologic form (with or without the presence of the inclusions), and the latter defines the characteristic bullet-shaped virus.
- Absence of history of animal contact has been reported in more than 30% of fatal cases of rabies. Here, also, it is the unquestioned association between the Negri body and rabies that constitutes the sole ground for a definitive etiologic diagnosis. The latter report is remarkable for the absence of history of animal contact and the occurrence of the fatal illness one week after vaccination for smallpox. Even in the presence of history of animal contact, it should be remembered that such an association is unwarranted as the behavioral alterations in the animals are not pathognomonic of any one disease.
- It is conceivable that the failures of antirabies therapy and the occurrence of false negative immunofluorescent results are related to the non-specificity of the Negri body for rabies.
- In no other viral disease is the light microscopy alone an accepted method for the definitive etiologic diagnosis of a disease.
The validity of the present observations needs confirmation by other observers and the answer will be found “not by dogma or skepticism but by open-minded uncertainty.”
doi: 10.1001/archneur.1975.00490440025002.
In Summary:
- According to the Institut Pasteur, Louis Pasteur’s initial efforts to isolate the rabies “virus” proved unsuccessful as the “virus” remained invisible
- The “virus” was not seen until almost a century later, in 1962, with the advent of electron microscopy
- Louis Pasteur had the idea of inoculating part of a rabid dog’s brain directly into another dog’s brain, causing the inoculated dog to subsequently die
- Inoculation with saliva (where the “virus” is supposedly found) was found to be a method which did not always produce rabies and symptoms did not declare themselves for months
- Pasteur accordingly inoculated a number of animals subcutaneously with some of the brain substance from other animals which had died of rabies
- Most of those inoculated developed rabies, but not all
- Pasteur’s idea of introducing into the brain of experimental animals some of the nerve tissue from an animal which had died of rabies was based on the principle (i.e. assumption) of providing the causal organisms with the nutritive medium best suited to their requirements
- There is a very high degree of uncertainty in the correlation between animal bites and the subsequent appearance of rabies-even when the biting animal is certifiably rabid
- While the mortality of clinical rabies is “virtually 100 percent,” the threat of death from the bite of a rabid animal is vastly less
- Estimates of the risk of contracting rabies from the bites of animals known to be rabid range from as high as 80 percent to as low as 0.5 percent
- Pasteur himself estimated that 16 percent of those bitten by rabid dogs would eventually die of rabies unless they submitted to his new treatment
- In 1887, the English Commission on Rabies drew attention to the uncertainty of all statistics on rabies citing:
- The difficulty of establishing that the attacking animal had in fact been rabid
- The variable effects of the location and depth of bites
- Differences in the lethality of rabid animal bites in different species and races
- The possible prophylactic effects of cauterization or other treatments applied to bitten victims before they submitted to Pasteur’s treatment
- The commission also suspected that at least one man may have died as a direct result of the Pastorian injections, and in the end it favored strict regulations on potentially rabid animals (muzzling and quarantine) over Pasteur’s more drastic remedy
- The great majority of the victims of rabid animal bites could forgo Pasteur’s treatment without experiencing any untoward consequences in the future
- Pasteur himself later pointed out some of the uncertainties surrounding the diagnosis of rabies
- Pasteur cited two cases in which symptoms of the disease had been induced solely by fear without any animal bite as well as another case which was induced by alcoholism
- Pasteur had a vested interest in emphasizing the difficulty of diagnosing rabies as he was then defending himself against allegations that his rabies vaccine not only sometimes failed to protect those who submitted to it, but in some cases was itself the cause of rabies and therefore death
- In defense of his vaccine, Pasteur now emphasized the extent to which symptoms like those of rabies could appear in patients who did not have the disease
- According to the CDC, the diagnosis of rabies can be made after detection of rabies “virus” from any part of the affected brain, preferably the brain stem and cerebellum
- The test requires that the animal be euthanized
- According to biologist Harold Hillman: “Killing an animal changes its biochemistry grossly. For example, its blood carbon dioxide, phosphate, lactate, and potassium ion concentrations, rise, while its oxygen, sodium ion, adenosine triphosphate, phosphocreatine, concentrations go down. These changes affect much of the tissue metabolism.”
- Hillman felt that “it is worth asking whether cell biologists should use tissues in vitro at all”
- The current “gold standard” test used to detect the “virus” on the brain tissue is the direct fluorescent antibody test (dFA)
- The dFA test is based on the “observation” that animals infected by rabies “virus” have rabies “virus” proteins (antigen) present in their tissues
- Because rabies is present in nervous tissue (and not blood like many other “viruses”), the ideal tissue to test for rabies antigen is brain
- When labeled antibody is incubated with rabies-suspect brain tissue, the story goes that it will bind to rabies antigen and unbound antibody can be washed away so that areas where antigen is present can be visualized as fluorescent-apple-green areas using a fluorescence microscope
- According to the CDC, during the 50 years the direct fluorescent antibody (DFA) test has been used in the United States, there has been no indication it has failed to provide accurate clinical information on the rabies status of an animal for the purposes of treating an exposed person
- The CDC states that because of its high sensitivity and specificity, in comparison to “virus” isolation methods, the DFA test is the “gold standard” diagnostic method for rabies (way to shoot “virus” isolation in the foot there CDC…)
- During clinical disease, millions of “viral” particles may be found intermittently in the saliva (which makes one wonder why they must kill an animal and do indirect antibody tests on decomposing brain tissue for diagnosis rather than properly purify and isolate the “virus” directly from the saliva supposedly containing millions of these entities)
- In theory, only a single rabies particle or “virion” is required to result in a productive infection
- The dFA results are based upon the opinion of an interpreter who uses an antigen fluorescence intensity and distribution scale from +4 on down to +1 to determine one of four conclusions: positive, negative, unsatisfactory, or inconclusive
- The dFA test has the disadvantage of poor sensitivity, and its specificity varies widely due to the subjective interpretation of test results
- DFA has several drawbacks such as:
- The need for an expensive fluorescent microscope
- Well-trained personnel
- Quality controlled reagents (antibodies, conjugates)
- Varied parameters used during microscopy
- Incubation times and temperatures
- The subjectivity in interpretation of the test results
- According to a 2017 study testing and reviewing dFA with the help of numerous labs, the results indicated that although all laboratories can perform the direct fluorescent antibody test, there are substantial differences in the overall results and test interpretation
- The authors stated that conclusive rabies diagnosis can only be achieved by appropriate laboratory testing as clinical and epidemiological diagnosis is challenging and leads to under-reporting
- The agreement between the laboratory results and those of the CDC, as measured by the sensitivity, specificity, concordance and kappa values:
- Only two laboratories correctly identified all samples tested (sensitivity and specificity of 1.0)
- However, 30% (7/23) of all laboratories reported at least one false positive and 83% (19/23) of all laboratories reported at least one false negative sample
- The average sensitivity was 76% with a range of 40% to 100%
- The average specificity was 88% with a range of 22% to 100%.
- While a majority of the laboratories had low false positive rates, there were considerable differences in the sensitivity
- The mean concordance was 81% with a range of 50% to 100% and the mean kappa score was 0.56 with a range of 0.02 to 1.00
- The level of concordance between the 23 participating laboratories and the CDC panel showed large variability
- Two laboratories had 100% concordance, while 91% of the labs had at least one discordant sample, with a total of 26 false positive and 61 false negative results among all laboratories
- The type of conjugate may also affect the sensitivity of the DFA test (monoclonal cocktail versus polyclonal, in-house made versus commercial)
- A study of 12 rabies reference laboratories in Europe demonstrated that the variability of conjugates could potentially lead to discordant results and influence assay sensitivity
- Another method for diagnosing rabies is the “isolation” of the “virus” by tissue or cell culture
- “Virus isolation” may be necessary to confirm inconclusive results in dFA/dRIT and for characterization of the “virus” strain
- In neuroblastoma cells, rabies “virus” grows generally without cytopathic effect
- In a bit of cirular reasoning, it is necessary to use dFA to confirm the presence of rabies “virus” by way of cell culture whereas cell culture may also be used to confirm inconclusive dFA results
- After intracranial (in the brain…some things never change) application, rabies induces clinical signs in mice that are relatively typical but have to be confirmed by dFA (i.e. the mouse that has had toxic cell culture goo injected into its brain causing symptoms must then be killed to have its cell-culture damaged brain examined by dFA to confirm the infection)
- Histologic examination of biopsy or autopsy tissues looking for signs of encephalitis is occasionally useful in diagnosing unsuspected cases of rabies that have not been tested by routine methods
- However, this method is nonspecific and not considered diagnostic for rabies
- Before current diagnostic methods were available, rabies diagnosis was made using this method and the clinical case history (i.e. non-specific and not suited for diagnostic methods were used to identify rabies for most of the 19th and 20th century)
- Histopathologic evidence of rabies encephalomyelitis (inflammation) in brain tissue and meninges includes the following:
- Mononuclear infiltration
- Perivascular cuffing of lymphocytes or polymorphonuclear cells
- Lymphocytic foci
- Babes nodules consisting of glial cells
- Negri bodies
- In 1903, Dr. Adelchi Negri reported the identification of what he believed to be the etiologic agent of rabies, the Negri body
- In his report, he described Negri bodies as round or oval inclusions within the cytoplasm of nerve cells of animals infected with rabies
- While this was the main method of diagnosing rabies for over 60 years, the presence of Negri bodies is variable
- Histologic staining for Negri bodies is neither as sensitive nor as specific as other tests
- Some experimentally-infected cases of rabies display Negri bodies in brain tissue; others do not
- Histologic examination of tissues from clinically rabid animals show Negri bodies in about 50% of the samples
- In other cases, non-rabid tissues have shown inclusions indistinquishable from Negri bodies
- Because of these problems, the presence of Negri bodies should not be considered diagnostic for rabies
- Despite these problems, until the mid-1960’s the diagnosis of rabies in the laboratory was based entirely upon the microscopic demonstration of Negri bodies and upon animal inoculation
- According to a study from 1942, the demonstration of Negri bodies was the method of choice since the diagnosis can be thus made in a few minutes or hour
- However, the authors admitted that the difficulties in demonstrating Negri bodies arose from two sources of error which could be enumerated as the inability to differentiate them from other inclusion bodies and cell structures, and inherent deficiencies in the methods of examination
- Every experienced microscopist has encountered the difficulty of deciding whether the bodies observed in some preparations are Negri bodies or cytoplasmic structures normal to the cell or if not normal at least only distorted cellular structures
- In the study of 84 cases of rabies proved by mouse inoculation they found Negri bodies only in the hippocampus 8 times and only in the cerebral cortex 4 times
- The authors determined that the finding of eosinophilic bodies in any portion of a brain from an animal suspected of having had rabies creates a doubt as to the diagnosis
- From their results it appeared that by microscopic examination of sections and in some smears, they were able to demonstrate eosinophilic bodies resembling “lyssa bodies” and atypical Negri bodies which are not associated in the brain with rabies “virus”
- Also the results showed that brain specimens in which the microscopic examination leaves the diagnosis in doubt contain rabies (i.e. they determined that injecting mice in the brain caused rabies without finding Negri bodies)
- The bodies that cause this confusion in the microscopic diagnosis of rabies are similar to ones found in certain parts of the brain of normal cattle and other animals and to atypical or small Negri bodies
- In a 1975 study, it is stated that rabies is the only “virus” that can be diagnosed by light microscopy based on the universally accepted conviction on the specificity of the Negri body for rabies
- However, the authors presented a case of a patient without rabies as determined by negative immunofluorescent study results for rabies and the absence of the rabies “virus “within the Negri bodies (light microscope) as demonstrated by electron microscopy
- Such an observation was inconsistent with the specificity of the Negri body in signifying the presence of rabies
- The result of this universally accepted dogma led to every instance in which a “Negri body” was seen being diagnosed as rabies irrespective of the circumstances
- Except for the occurrence of the Negri body, rabies encephalitis does not have any pathognomonic clinical or pathologic features (i.e. non-specific and overlapping symptoms associated with many diseases)
- Variola-vaccinia (Smallpox) “virus,” for example, can produce the same clinical pictures
- There is remarkable variability in the intensity of cellular inflammatory response in rabies encephalitis
- The diagnostic efforts in the past have been mainly directed to the “specific” finding of the Negri body
- The absence of Negri bodies in a substantial number of fatal cases of rabies and the remarkable lack of inflammatory response in some instances of the disease signify the importance of obtaining a careful history
- Absence of history of animal contact has been reported in more than 30% of fatal cases of rabies
- In these cases, it is the unquestioned association between the Negri body and rabies that constitutes the sole ground for a definitive etiologic diagnosis
- Even in the presence of history of animal contact, it should be remembered that such an association is unwarranted as the behavioral alterations in the animals are not pathognomonic of any one disease (i.e. there are many diseases which are said to cause the same symptoms in animals)
- It is conceivable that the failures of antirabies therapy and the occurrence of false negative immunofluorescent results are related to the non-specificity of the Negri body for rabies
- In no other “viral” disease is the light microscopy alone an accepted method for the definitive etiologic diagnosis of a disease
- The author concludes that the answers to the observations made will be found “not by dogma or skepticism but by open-minded uncertainty.”
When one looks into the history of rabies and the methods used to diagnose the disease, it becomes undeniable that the mythical status that surrounds this fear-based fictional narrative fed to the masses throughout the centuries is entirely unjustified and unwarranted. There is literally nothing there in support of rabies as a distinct disease caused by a specific “virus” that is transmitted to humans through the bite of a sick animal. If we were to lay out the facts in front of a jury, it would be an easy conviction:
- The pivotal moments of discovery in the late 19th century were built upon the fraudulent foundations laid out by Louis Pasteur, a man who manipulated and massaged his own data in order to sell his theories and his vaccine for fame and fortune.
- The supposed “isolation” of the “virus” didn’t even take place until nearly a century after Pasteur admitted to never identifying a causative agent and yet it missed the necessary requirement of showing any indirect evidence of the “virus” highjacking the cell as the culture lacked any evidence of the cytopathogenic effect.
- The actual correlation between animal bites and symptoms of disease was considered highly uncertain and those who were attacked and bitten by clearly rabid animals could easily forgo any treatments without any ill health effects.
- The incubation period for the disease is inconsistent and is said to range anywhere from 6 weeks on up to 25 years before the development of symptoms.
- The severe symptoms associated with rabies are a rare occurrence in nature and are in fact seen most frequently as an adverse reaction to the vaccine said to contain neurotropic ingredients.
- The acknowledgment by Pasteur of “false rabies,” which was said to be brought about solely by FEAR of aquiring the disease as well as alcohol and/or drug use, was used to take attention away from his vaccine causing injury and death.
- The statistics regarding rabies cases were considered unreliable due to the lack of any specifuc disease-defining symptoms as many diseases in animals and humans mimic the clinical picture.
- The diagnosis of rabies, for much of its history, relied upon clinical symptoms and the histopathological findings related to encephalitis and Negri bodies, all of which are non-specific and are not suitable as a diagnostic measure for the disease, thus calling into question any case statistics related to rabies.
- The only way to claim pathogenicity of the “virus” is by way of the completely unnatural route of intracranial inoculation of diseased brain and nervous tissues directly into the brains of dogs and mice.
- The more recent modern method of direct fluorescence antibody tests, considered the “gold standard” diagnostic test, is claimed to be highly sensitive and specific, yet the results of the tests are open to human interpretation and have been shown in reviews to have low sensitivity and varied specificity.
The narrative surrounding rabies is based upon many primal fears. It plays on the fear of death, the fear of the unknown, and the fear of mutilation. Just like the rabid animal lurking in the shadows ready to strike, the “virus” hides inside the body once infected, waiting for the right moment to unleash a painful and excruciating death unless the infected leaps for the miracle cure in time. If they are a moment too late and the symptoms set in, it’s game over. This same scenario is regularly sold to the masses in our daily entertainment with the recent zombie craze. One must be afraid of the bite. Once bitten, the “virus” takes hold and the victim is condemned to certain death.
However, just as Louis Pasteur recounted tales of the fearful succumbing to the exact same symptoms in absence of any animal bite, we must realize that the real enemy here is not a “virus” but an ingrained fear that stems from outdated and unproven fictional narratives. Moreso than any of the other more common diseases of the time such as smallpox and syphilis, rabies was the perfect mascot to convince the doubting public that disease-causing pathogens exist, can be transmitted, and can be prevented by way of vaccination. The imagery of the dirty mangled dog stumbling down the road, frothing at the mouth and seeking its next victim to transfer its parasitic contents into was a powerful visual tool for pathogens that remained nothing but formless thoughts at the time.
However, the evidence consistently shows us that there is no dangerous invisible entity waiting in the wings inside the saliva of a rabid animal looking to seep into the open wound of a bite mark. There is no reason for any victim of an animal attack to subject themselves to the toxic treatments based upon the fear of an impending gruesome death. Just as there are no zombies coming for your brains, there is no frothing rabies “virus” looking to do the same. The foundation for germ theory and vaccination established by Pasteur was never built from any purified and isolated “virus” shown scientifically to exist in nature. It was built upon the only “virus” that has ever truly existed: the “virus” of fear.
For an excellent breakdown of the rabies fraud, please see Dr. Sam Bailey’s What About Rabies? video:
[References for Dr. Sam Bailey video “What About Rabies?”]
- Corona Investigative Committee, “Session 90: The Virus Of Power”, 5 Feb 2022.
- AVMA, “Rabies surveillance in the United States during 2019”.
- CDC, “Rabies”.
- CDC, “About Rabies”.
- Wikipedia, “Rabies virus”.
- Dr Sam Bailey, “Electron Microscopy and Unidentified ‘Viral’ Objects”.
- Wikipedia, “Joseph Lennox Pawan”.
- Dr Joseph Pawan, “The Transmission of Paralytic Rabies in Trinidad by the Vampire Bat”, 1936.
- “Rabies: interactions between neurons and viruses. A review of the history of Negri inclusion bodies”, 1996.
- Gerald Geison, “Pasteur’s Work on Rabies: Reexamining the Ethical Issues”, 1978.
- Dr Montague Leverson, “English City of Leicester as example of benefits of abolition of vaccination”, 1909. Available as an E-book download here
- Mike Stone, “Louis Pasteur’s Unethical Rabies Fraud”, 25 Feb 2022.
- “Tetrodotoxin, an Extremely Potent Marine Neurotoxin: Distribution, Toxicity, Origin and Therapeutical Uses”, 2015.
- Blindsided by Rabies with Michael Wallach on the Skeptico Podcast
cover image credit: Prawny